When Single Payer becomes the law of the land, Medicaid will be the foundation.
We’ve looked at the current push for Medicare for All, the factors that I believe will drive us to some form of single payer, and posted a primer on Medicaid.
Here’s why it’s going to be Medicaid for All.
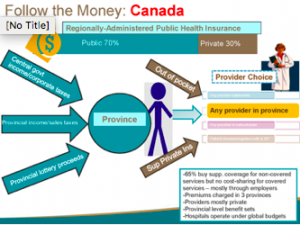
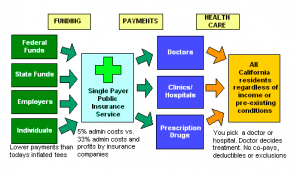
- Medicaid for All will spread the cost of universal coverage across states, reducing federal financing requirements.
Medicaid is a state AND federal program; States provide a lot of the funding for Medicaid; on average the Feds contribute 63% and states 37%. This is critical, as Congress will want to spread the cost of a Single Payer solution and there’s no better way to do this than require states to pony up big dollars [State contributions vary based on a state’s average personal income relative to the national average; states with lower average personal incomes get more federal dollars.] - Medicaid is already built to cover everyone.
Medicare covers people of all ages, Medicare is very much elder-care focused.
Adapting Medicare to handle everyone from newborns to elderly, maternity care to pediatrics will be difficult, time-consuming, and expensive. Medicaid does all this and more – today. - Generally, Medicaid is less expensive than other “systems”.
This is due to much lower provider payment and significantly lower administrative costs. Yes, this means providers are going to be paid less. - Medicaid member satisfaction is pretty good; access to care is not much of an issue.
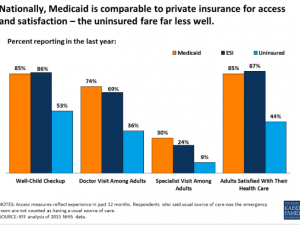
- Medicaid-based Exchange programs are much more successful in the Exchanges than commercially-based plans.
The Centenes et al [Medicaid-based plans] understand the demographics of the uninsured, have lower medical costs, and already have provider networks, customer relations operations, workflows and processes set up and operational. At the end of the day, lower cost wins – and their costs are lower. - Medicaid is a simple, fully-integrated healthplan.
Medicare’s alphabet-soup of Parts A B C and D is confusing and convoluted, with different payers often covering the same individual. This increases administrative costs, member hassles, and decreases quality of care (co-ordinating pharmacy and medical care between different payers is problematic at best. - Managed Medicaid plans are working.
These plans currently exist in most states, and many have been able to deliver excellent care at lower costs through innovation and very tight focus on outcomes. One example is using paramedics to deliver care. [disclosure – I sit on the board of Commonwealth Care Alliance, a Massachusetts healthplan that serves dual-eligible members]
Tomorrow I speculate on how Medicaid for All will integrate with Medicare and employer-based coverage.
What does this mean for you?
Better care, lower costs, while a big impact on pharma, device companies, healthcare systems, and healthcare providers.


 Mr Gaffney, undated photo from facebook
Mr Gaffney, undated photo from facebook