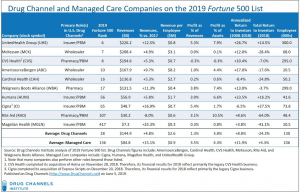
Monday’s news that giant TPA Sedgwick is acquiring York from Onex shouldn’t have surprised anyone. Sedgwick has been – and will continue to be – an acquirer. Posting revenues of $2.7 billion last year, the TPA’s recent growth – revenues increased by more than 50% in 2018 – has been driven largely by acquisition.
Bought by private equity firm Carlyle just last year for $6.7 billion (from KKR), Sedgwick’s value has likely tripled over the last few years. Of course, that growth required major expenditures, so it’s not like the owners didn’t invest a lot more than the original purchase price of the business.
Growth is critical to any private equity-owned company and in a highly mature industry the fastest, least expensive, and best way to grow is by buying competitors. VeriClaim and Cunningham Lindsey were two of the larger acquisitions during the last few years, and both were smart buys. They were strategic, adding different skill sets, customer types and service capabilities in addition to hundreds of millions to the top line.
The York acquisition follows the same game plan; it adds several key assets/capabilities;
- a highly profitable managed care unit built by former leader Doug Markham (York has it’s own proprietary bill review software…);
- a wealth of experience in program business management; and
- strong municipality and governmental entity offerings.
With international capabilities and claim handling expertise in all P&C lines, Sedgwick is positioned to grow by handling claims from extreme weather events driven by climate change. It is also gaining efficiency – which will lead to more growth – in shrinking lines such as workers’ comp.
While I’ve locked horns with CEO Dave North in the past, one has to respect the strategic vision, marketing prowess, and execution skill that has pushed Sedgwick to the top of the TPA industry. Senior management is capable indeed; there’s some solid talent at York that will make it even better.
Last point – and it is a critical one. Over the last decade there have been dozens of PE deals in workers’ comp and P&C services. Most private equity investments performed quite well despite – or more accurately partially because – they used debt intelligently.
One would do well to keep that in mind these days; in and of itself debt is not bad or harmful. What is “bad” is a faulty investment thesis and crappy execution.
What does this mean for you?
Strong leadership, management that can execute, and an industry-leading brand make for success.
How do you stack up?