WorkCompCentral hosted a webinar last week (you can watch at no cost) diving into key issues related to Florida’s experience with COVID19 and workers’ comp. Moderated by Rafael Gonzalez (one of the nicest people you’ll ever meet), the panel included a defense attorney, judge, and managed care executive providing different perspectives on COVID’s impact.
Most of the discussion focused on solutions; we’ll touch on the ongoing issue of claim acceptance before highlighting some of the solutions discussed by the panelists.
Claims filed v accepted
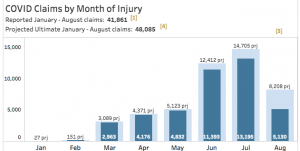
Judge David Langham noted that about 7,000 of roughly 17,000 COVID claims filed have been partially or completely denied, yet to date only a handful have filed petitions seeking benefits. (A petition would lead to a formal hearing.)
Ya’Sheaka Williams, a defense attorney, spoke at length about healthcare workers’ exposure, indicating that in her experience claims filed by these workers weren’t contested. She provided good insight into differences between “essential” vs “non-essential” workers, noting sanitation workers are even more important now than ever as it is critical to safely dispose of potentially contaminated materials.
Langham also noted that 96% of accepted cases have resulted in payments <$5,000; the average is <$1,000. (consistent with data Mark Priven and I previously reported)
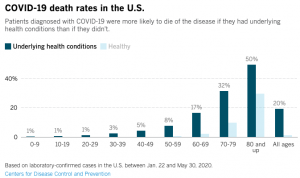
Of course, as Langham indicated we do NOT know what the long-term impact of COVID19 on individuals will will be; there’s evidence that some individuals have lasting chronic conditions, some of which can be quite debilitating.
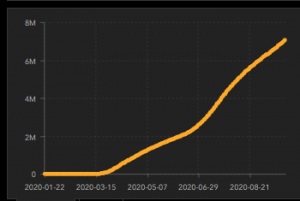
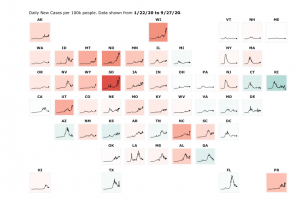
Langham averred “in the United States, we aren’t reporting who has recovered, whatever that means.” That surprised me, as a slide displayed earlier in the same presentation specifically reported recoveries in the US. (the picture below is from the same site, captured this morning)

In defense of Judge Langham, I hasten to add that in fact that while there is some reporting of “recoveries”, there’s no universally-accepted definition of “recovery”, nor is the reporting of recoveries consistent across states or even counties within states. For example, Texas has reported 680,000 “recoveries”, while New York – a state with much higher infection counts – has only reported 77,000, and California and Florida have not reported ANY recoveries. (at least as reported by JHU)
The lack of clear and specific definitions and guidance from the Federal Government – and a Federal mandate that reporting entities stick to those definitions and guidance – is highly problematic.
Matthew Landon, Chief Strategy Officer of MTI America, suggested employers ensure they are using the same processes, procedures, and strategies to evaluate COVID19-related claims that they use for all claims. Consistency is critical to demonstrate objectivity.
Lessons learned
Judge Langham noted that virtual hearings are proving we can use technology to speed up hearings, engage with claimants more effectively, and get to resolution quickly despite the inability to get together in person. He also encouraged all of us to “protect ourselves mentally and physically” so we can help others.
Kudos to Judge Langham for reminding us that before one can help others, one has to take care of oneself.
Landon identified telephonic translation services a key tool speeding up claims handling and ensuring the right care is getting to workers with language limitations. He also noted care within medical offices seems to be more effective as patients are seen more quickly with lower waiting times; office managers are working to keep the number of patients in offices as low as possible.
More care is being delivered in the home of late, a response to workers’ desire to avoid medical facilities.
Ms Williams reported Tampa Airport is partnering with BayCare Health Systems to provide passengers coronavirus tests on-site at no cost to the passenger, highlighting one example of companies working together to come up with creative solutions to reduce risk and personal stress levels.
She also was encouraged that the delays in accessing care experienced by many injured workers seem to have abated somewhat, a promising development as more clinical practices open up for on-site care and more providers adopt tele-medical solutions.
What does this mean for you?
Good information from folks with deep knowledge of Florida’s experience, much of it applicable to other states as well.
note MTI America is an HSA consulting client