The medical community is wrestling with ethical issues arising from vaccines.
Simply put, should unvaccinated people infected with COVID be treated differently than the vaccinated?
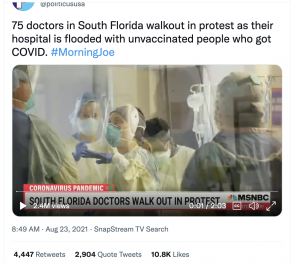
This isn’t just an academic exercise; here in the Upper Valley of New Hampshire and Vermont, emergency rooms, critical care units, ICUs and Pediatric ICUs are stuffed full of COVID patients, almost all of whom are unvaccinated.
The Governor has issued an Executive Order intended to give hospitals more flexibility in setting up overflow units. At least two NH hospitals have postponed or halted elective surgeries as a result of the latest COVID surge.
Michigan may be in even worse shape.
The implications are real and potentially tragic. Parents, friends, children or neighbors in car accidents, struck by heart attacks or strokes, suffering from kidney failure or pancreatitis or appendicitis or anaphylactic shock may find their local hospital doesn’t have an open bed and/or is operating short-staffed.
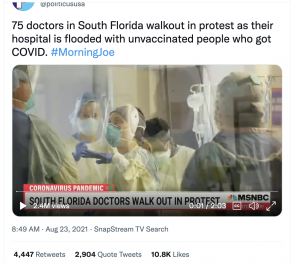
The latter is worsening by the day, as nurses, support staff, physicians and other clinicians are exhausted, frustrated, angry and despondent over long hours and the need to treat unvaccinated COVID patients. That and a relatively tiny number of healthcare providers have also bought into the lies perpetrated by antivaxxers, exacerbating the staffing shortage as they lose their jobs.
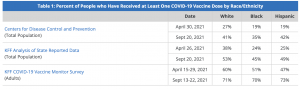
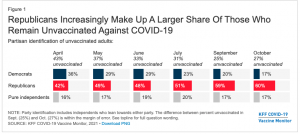
The exception to this discussion is for populations that have been mistreated, lied to, abused and misled by eugenicists masquerading as researchers.
The arguments for NOT treating those adults who are unvaccinated by choice (rather than due to a medical exemption) go like this…
- the “slippery slope” argument – once we do this, then we’ll
- refuse to treat obese people for heart disease, kidney disorders, diabetes, hypertension etc; smokers for heart disease, cancer or COPD; drinkers for liver disease – as if individual decisions with repercussions limited to that individual are the same as antivaxxers’ potential to spread infections, contribute to variant development and possibly kill family members, kids, health care workers and co-workers in the process.
- as long as we’re talking about obesity…it isn’t
- communicable,
- preventable by vaccination, or
- filling ICUs to over-capacity.
- the false equivalency argument –
- refusing to treat the “unvaxxed by choice”? than you shouldn’t provide care to women who have unplanned pregnancies – as if a one-time event is equivalent to a person’s brazen willingness to potentially infect dozens of us.
- the “you are violating my freedoms” argument
- if we can ban smoking in schools, restaurants, offices, airports and public transportation, we can certainly require immunization and penalize those without valid exemptions (if you think you should be “free” to smoke in a school or medical facility, that’s a whole different issue)
- Oh, and pets are required to be immunized against dangerous diseases, as are kids.
Which leads us to the facts vs beliefs issue.
“Beliefs” – that you are a better driver than anyone else so should be allowed to drive at twice the speed limit through a school area and your child doesn’t need to be in a child safety seat and you don’t need to wear a seatbelt and you can hold your liquor so driving buzzed isn’t a problem for you; that you know more than 99% of the experts so you won’t get vaccinated, that children don’t die of COVID are NOT facts.
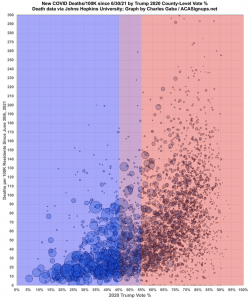
And when those beliefs are demonstrably false – as the anti-vaxxers’ arguments clearly are – the moral dilemma becomes more complicated.
“Freedom” isn’t free – if you want to be free to be unvaccinated, then you – no one else but you – have decided to accept the consequences of that decision.
Actually, that’s not right – because your decision is directly affecting your neighbors, family members, and co-workers. It is directly affecting my family members who work in healthcare, people you will infect, and lives you will disrupt.
In fact, freedom from disease, from economic disruption, from grief when loved ones die – comes at a cost – and that cost – however slight – is all of us getting vaccinated.
What does this mean for you?
Spare us the false equivalencies, the slippery slopes, the my freedoms nonsense, get the damn vaccination and wear a damn mask.
And when you get COVID, stay home and don’t interfere with our freedom to be free of COVID.
A more comprehensive discussion of the arguments against vaccination is here.