Back to NCCI…didn’t want to overload your inbox last week.
For anyone who has heard Bob Hartwig PhD speak, he violates all the common rules about presentations and presetting – and is excellent nonetheless. Methinks it is because Bob is both deeply knowledgeable and enthusiastic beyond measure.
On to the content.
In the overall P&C market, we’ve just had three consecutive years of underwriting profits, an occurrence previously experienced 45 years ago. Back in the days before 1970, underwriting profits were common, primarily due to the low investment returns available in those days.
One of the key drivers has been continued reserve releases as insurers and employers take down reserves, adding to gains.
Bob noted there’s been wide disparity among and between states in terms of premium increases, linked quite closely to each state’s underlying economy, but overall premium growth has been pretty modest. With organic growth somewhat stalled, insurance M&A activity ramped u significantly in 2015 – not just in the US but in Asia and across North America.
Hartwig talked about the Trump v Clinton positions on matters of import to P&C insurers; see his presentation for the relevant slide.
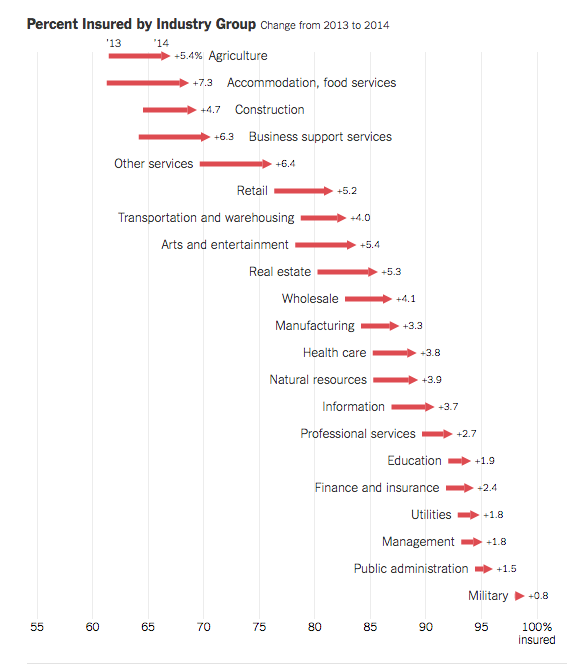
Non-farm payroll is increasing at about a 4.5% annual clip since the great depression – due to higher employment, higher pay rates, and more hours. This is GOOD NEWS INDEED. There are also early indications that labor force participation has improved “modestly” since the beginning of 2016, and the number of “discouraged workers’ has also dropped significantly of late.
Manufacturing is a major issue in workers comp – while there’s been solid growth since 2009, it is contracting in the energy sector along with the entire non-durable sector.
The on-demand aka Gig economy – there are a plethora of regulatory issues which, in turn, have implications for insurance. Independent contractor v employee, private passenger auto vs commercial auto, liability, etc are all of major concern. Notably, young, minority urban males are the most likely to offer gig services – this demographic group is also more likely to incur an occupational injury. And, gig workers WANT more regulation – they seem to think of themselves as employees.
The sharing economy is going to have hugely disruptive effects on insurance; no longer does one entity own the asset that delivers the service or product, distributes it, services it, and employs those who do the work. This will require a rethinking of how and what is insured, and how “claims” are assessed/attributed/reported/paid.
Very glad there’s lots of smart millennials that can figure this out because it sure makes my head hurt.
41% of occupational deaths were due to transportation incidents – almost 2000 in 2014, 60% of those caused by roadway incidents. Of course, that’s not the good news, what is the good news is increasingly-automated driving will likely reduce the death rate dramatically. The “single greatest area where we can see a decrease in frequency of deaths due to improved automation.” (paraphrase, it’s impossible to type as fast as Bob talks)
Hartwig concluded with a discussion of the growing involvement of private equity and venture capital in the insurance industry. Google Compare came to the US from the UK; after a brief run it closed up shop in February this year due to low profit margins. When you have a hurdle rate (desired return on investment) of 18%, insurance is probably not a terribly promising industry.
Nonetheless, there are a plethora of insurance-related companies getting $10 million or more in funding to do something disruptive in P&C insurance. Distribution, analytics, data warehousing, insurance technology are all areas of focus.
And that’s it!