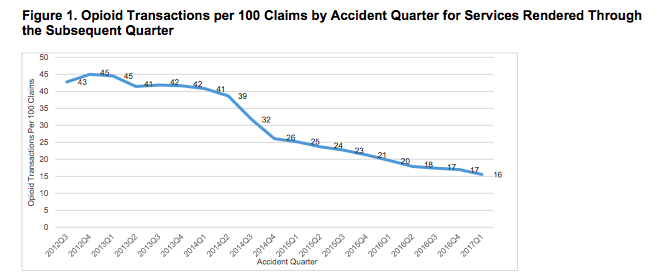
My best guess is about a quarter of those are work comp patients.
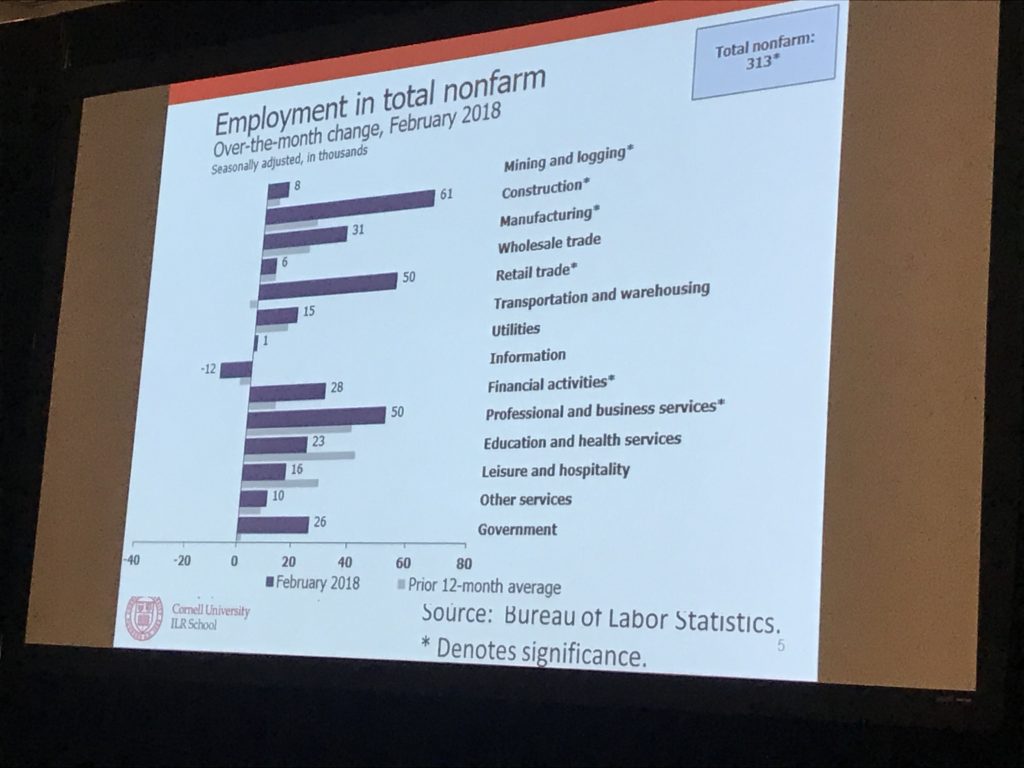
Opioid use disorder (OUD) drains the workforce of qualified, experienced workers, costing our economy $40 billion.
Healthcare costs for OUD alone were $28 billion in 2015 – and all but $2 billion of that was paid by insurance – mostly Medicaid (which is taxpayer funded).
If you are 50 or younger, you’re more likely to die from opioid use than anything else – not a car accident, not cancer, not a heart attack, not diabetes.
Solutions
Medication-assisted therapy (MAT)- using methadone, buprenorphine, vivitrol to help victims get off and stay off opioids – is, for most folks, a key part of recovery. Yet most states have far too few MAT facilities, and many facilities only provide one or two of those medications (not surprisingly, different people seem to do better on different therapies).
Yet there are far too few providers trained and able to provide MAT. From Inflexxion:
Data shows that less than half of privately funded treatment programs offer any form of medication-assisted treatment. That number falls to 23% in publicly funded programs. According to the 2013 National Survey on Drug Use and Health, of the 2.5 million opioid-dependent or opioid abusing Americans, fewer than 1 million received MAT.
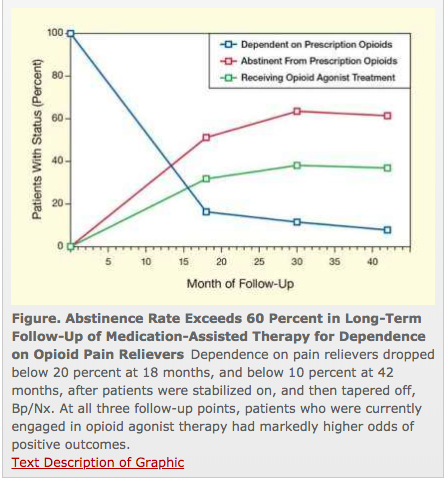
MAT, coupled with counseling and patient-centric, individualized treatment plan can be quite effective. A solid study found over well over half of patients using MAT were not using the illicit drugs 18 months into treatment – a remarkable success.
However workers’ comp payers are often unable to find MAT facilities, lack the understanding needed to develop a comprehensive, long-term treatment approach, and are loathe to go down that path, as they’re afraid it will make the employer liable for all manner of additional services.
What does this mean for you?
States can and should come up with novel ways of encouraging treatment while limiting future liability.
This will save thousands of lives and billions of dollars for employers and taxpayers.