Six weeks ago I predicted:
TPAs will add more business, mostly from carriers.
As work comp continues to shrink, insurers will ramp up efforts to shed assets and expenses to reduce their cost structure. By outsourcing claims, carriers are trading the high fixed costs of a claims infrastructure for the variable cost of a per-claim admin fee.
The smarter carriers will negotiate hard so they don’t get screwed by medical management and other non-fixed fees…but many carriers aren’t that smart…
and…Insurers will reduce staff, particularly in claims.
Here’s an update.
There’s been lots of rumors out there about AIG’s plans to get out of the claims business and associated layoffs, so I reached out to AIG. (full conversation below)
Net is I’m hearing there have been layoffs in IT (never a strong suit at AIG), work comp claims, and medical management services. Likely other areas as well.
Focusing on work comp/medical management, this is a) wholly predictable and b) likely to happen at other insurers.
The reasons are straightforward:
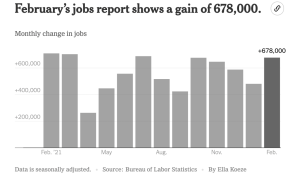
- work comp is a declining industry
- in 4 years there will be 10% fewer claims than there are today
- work comp is a classic cash cow; mature, throwing off lots of cash and stagnant
The implications are clear – why would an insurance exec invest in a business that is declining, way behind in technology investment, has an aging workforce and can’t attract young talent?
Especially when it can outsource claims to a TPA, thereby:
- reducing fixed costs and unallocated loss adjustment expense (ULAE)
- eliminating the need to invest in IT upgrades for claims and medical management systems
- getting rid of an older and expensive workforce and the attendant costs for real estate, IT support, telecom, benefits and on and on.
Congratulations to Gallagher Bassett, which appears to have landed a lot more work. This will help GB immensely as it will gain revenue it can use to make those IT investments, hire and train staff, and upgrade operations.
Finally, corporate-speak.
Why AIG would not answer questions clearly and cogently is beyond me. Without those answers, one has to look to message boards and contacts at the company and those recently departed, sources that have – by definition – more narrow perspectives influenced and affected by the impact of AIG’s actions and non-actions.
That doesn’t mean those perspectives aren’t valid – not at all. It does mean that you, dear reader, don’t have the full picture as to what is happening at AIG and why.
What does this mean for you?
If AIG work comp is a customer, pay very close attention.
Email conversation:
here’s what I asked AIG
I’m working on a blog post re carriers using TPAs for workers’ comp claims. I understand AIG is in the process of outsourcing WC claims to Gallagher Bassett; evidently there was an internal communication to employees in December addressing this.
My questions:
-
-
-
- AIG has long used TPAs for claims handling, but also handled claims internally. Is AIG in the process of outsourcing all/most WC claims that were previously handled internally?
- If so, what is driving this decision?
- Sources indicate the timing is Q2 2022; is this accurate?
- Indications are AIG is also reducing the role of HDI; can you speak to that?
Here’s AIG’s response:
AIG has entered a strategic partnership with Gallagher Bassett for the shared management of our “bundled” workers’ compensation claims in the U.S. This partnership will combine AIG’s in-house claims expertise and customer service with Gallagher Bassett’s industry-leading infrastructure, analytics and technology. AIG will continue to handle major loss and specialty claims and medical management, while also providing technical and strategic guidance for all claim management and resolution.
And here’s my follow-up
So, thanks for the statement.
Is AIG staff handling claims?
Is AIG doing all the Managed care work but using GB’s IT for claims?
My understanding from AIG staff is that GB will handle claims, so I’m a bit confused.
AIG’s response was classic corporate-speak and – as you can see – didn’t answer my questions. AIG also didn’t respond to my follow-up.