It’s just a couple weeks before WCRI’s annual meeting…in Phoenix’ warm and sunny clime. Register here – and do it now as this always fills up.
Unlike other events, attendees are mostly senior management leaders and the like; lots of expertise and experience all in one place makes for a very productive couple of days…
I caught up with WCRI’s John Ruser PhD and Andrew Kenneally to get their take on some of the topics…
MCM – Dr Autor – The implementation of the Biden administration’s IRA, infrastructure, CHIPS and other legislation is ramping up; where does Dr Autor see the direct and indirect impacts of this legislation on workforce, employment, and compensation?
JR – Dr Autor is a great speaker, and has won prestigious awards including one of the top prizes in labor economics, the Sherwin Rosen award. He is going to take a longer-run view, discussing the evolution of work. Dr Autor will be talking about how tech and AI will affect the future of work and the way work is done. One question to be addressed: “is tech substituting for (replacing) or supplementing workers?”
MCM – The medical inflation topic is top of mind for many…what will Dr Fomenko and Dr Yang be addressing?
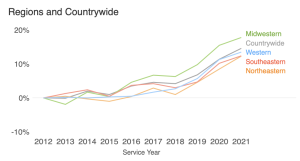
They will be building on work they’ve done in the past on the design of fee schedules and WCRI’s own price indices to show how inflation manifests itself and how system features can serve to control medical inflation. The focus will be on medical payments, provider prices and the impact of fee schedules.
MCM – Very happy to see climate change on the agenda; what drove WCRI’s decision to give this topic the stage?
JR – Clearly we are seeing the impacts of climate change in the form of stronger storms, hurricanes and rainfall, these and others are affecting workers comp. This session is a no brainer as the direct impacts are pretty obvious.
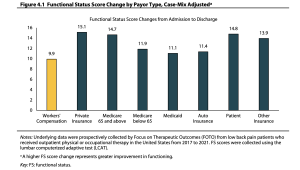
MCM – Physical Medicine is has been somewhat of a concern for payers as costs are trending slightly upward along with utilization. What are some of the drivers of this increase?
JR – Drs Wang and Mueller will look across states and at factors that are associated with the extended use of physical medicine beyond guideline “limits”. They will identify some factors that are associated with extended physical medicine; some obvious like severity and others less so – such as whether there are multiple providers of physical medicine services and issues around coordination of those services.
JR -Finally, we are really pleased at the mix of our own research and panel discussions with a diverse group of stakeholders (unions, providers and employers, regulators and insurers), all of whom bring deep expertise to the discussion.