Summer’s arrived in upstate New York – and boy do we appreciate it. While I was watching all the trees turn green, I missed reporting on a bunch of stuff last week.
So better late than never, here it is.
P&C industry outlook
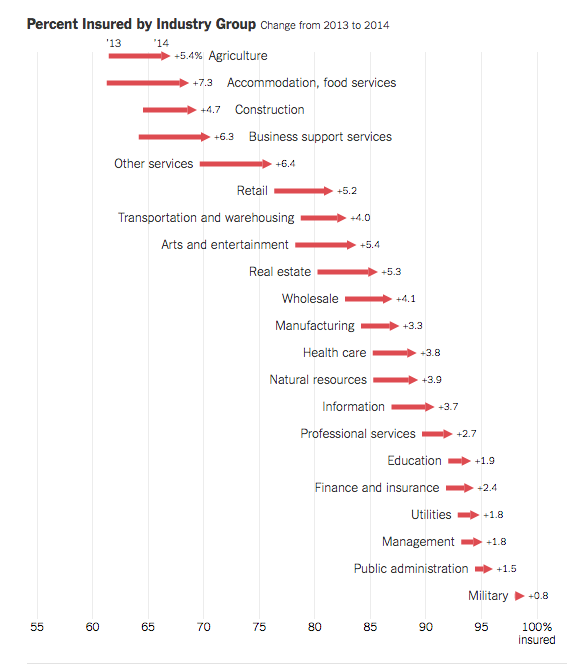
Let’s start with the macro stuff. A couple weeks back, Fitch published a piece wherein they opined the P&C industry is in for a tough time this year. After several years of stellar performance, Fitch expects prices to decrease as competitors battle for market share. Here’s how they put it:
Renewal rates are flat or declining for most commercial market segments following a hardened market from 2011-2014. The price competition comes from underwriting success and market capacity expansion from earnings accumulation. As price competition intensifies however, this will likely be a drag on premium growth, according to Fitch. Commercial lines written premium volume grew by only 1.8 percent in 2015.
For work comp, Fitch identified prescription drug costs and continued low interest rates as problematic; the first increases costs while the second reduces investment income.
Opioids
The number of opioid scripts in the US actually declined last year. And that was the third year in a row. That’s the best news we’ve heard in quite a while. Since 2012 – the peak year for opioid script volume – the number of scripts has dropped by 12% – 18% (depending on the data source).
In case you’re interested, prescription opioids accounted for about $10 billion in total spend in 2015. Workers comp accounted for around 14% of that, a rather striking figure when you consider total work comp medical spend accounts for 1.4% of overall US medical spend.
Yup, work comp uses about ten times more opioids than other payers.
And how the bad news; the drop in scripts hasn’t been accompanied by a decrease in the death count, which stands at 28,000 for 2014.
California Workers’ Comp
Well, at least it hasn’t gotten any worse. That’s my take on the just-released CWCI study on the UR/IMR process for Q1 2016.
- IMR volume is about the same as last year at 160,000 determination letters per year;
- the overall IMR uphold rate is the same as last year at 89%;
- Rx drug requests still account for nearly half of all disputed medical service requests submitted for IMR (and 40% of the Rx drug IMRs are requests for opioids or compound meds);
- and a small number of docs still account for the majority of the disputed service request that undergo IMR (the top 10% of medical providers accounted for more than ¾ of the IMR service requests).
My take – the IMR process is preventing people who don’t need opioids from getting scripts for opioids. That’s a very, very good thing. Yet the same docs keep prescribing this crap to patients knowing full well these requests will be rejected.
I’m very much looking forward to hearing all those “injured worker advocates” heaping praise upon the system for protecting their clients’ health and wellbeing, and that of their kids as well.
I’ll personally nominate each of them for a Comp Laude Award.