For decades WCRI’s CompScope reports have provided deep insights into workers compensation in many states. The information is germane not only to those focused on specific states, but for anyone looking to understand what works and what doesn’t, how regulatory changes affect stakeholders, and how systems adapt to those changes.
The latest versions are the 21st edition, adding new depth and detail. Streamlined access to specific information and data via quick tabs is a big plus.
I took a deep dive into WCRI’s Florida report, and came away with two key takeaways.
- If you are a facility, you should love the fee schedule.
- If you are a medical provider, you should hate it.
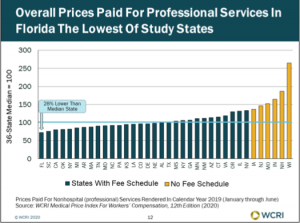
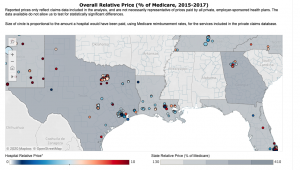
Medical providers – docs, PTs, specialty providers – are paid about 30% less than the median state, with PTs at 28% less, E&M codes at 21% less, and x-rays reimbursed at a rate 45% less than the median.
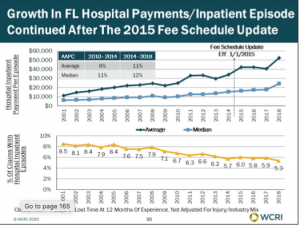
Hospitals are making huge bucks off workers comp – especially for inpatient visits. Recent data indicates well over half of all inpatient episodes are “outliers”. Once claims incur more than $59k in charges, reimbursement switches from per diem to percent of charges, more accurately known as “license to steal.”
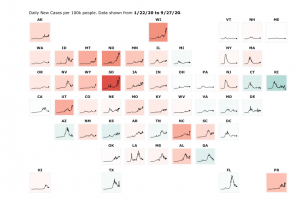
I get why hospitals are desperate to make huge dollars charging Florida’s employers and taxpayers outrageous amounts: the state didn’t expand Medicaid and has the second highest percentage of non-elderly folks without health insurance (Texas is tops).
Florida hospitals have to treat a lot of folks without health insurance, and they are looking to workers’ comp to help pay for that treatment.
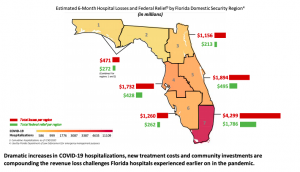
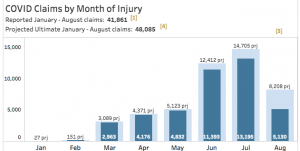
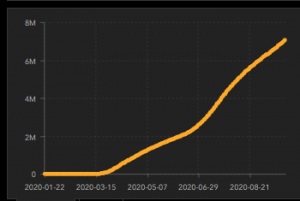
Oh, and COVID’s fallout is adding to hospitals’ financial woes. (take the info above with a grain of salt; it was put out by the Florida Hospital Ass’n.)
The result – hospitals are getting killed financially.
What does this mean for you?
Make time to read and understand solid research. It will determine your future.