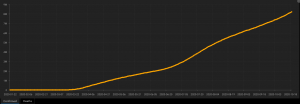
A solid study found that the US infection rate is likely way higher than the official reports. The brainiacs at The Economist estimate almost one in every five of us has had the disease.
Coincidentally, I was talking with a client yesterday about his bout with what sounded a lot like COVID. Turns out his wife had it as well. This is just one of several stories I’ve heard from folks who got sick as far back as last December or January.
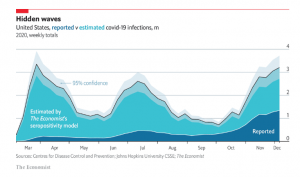 The Economist has a very well done COVID tracker that provides data on excess deaths during the pandemic era, as well as a description of potential reporting issues and causes.
The Economist has a very well done COVID tracker that provides data on excess deaths during the pandemic era, as well as a description of potential reporting issues and causes.
Before you scoff, read the article; the evidence is compelling that the pandemic has led to many more deaths than expected.
A study examining hospital readmission rates for COVID patients found more than a quarter died or returned to the hospital after their initial discharge. This sounds pretty high, but it is actually lower than longer-term death and readmission rates for heart failure and pneumonia patients.
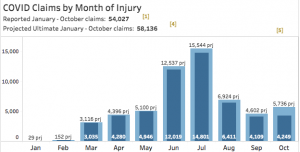
Thanks to WorkCompWire for the piece on CWCI’s report on claims for public self-insureds for the fiscal year ending June 30, 2020. Recall that COVID hit California in early March, so the reports’ findings reflect 8 months of a “normal” year and 4 pandemic months. Top takeaways:
- Claim counts dropped over 6%
- Indemnity expenses zoomed up almost 17%.
My view – it is highly likely the pandemic drove increased disability duration as patients couldn’t access care, facilities postponed elective procedures, and newly-injured workers found it harder to get appointments.
You’ll likely hear much more in a few months if you Save the Date for CWCI’s Annual Conference – on Thursday, March 11, 2021 the brilliant minds and best-presenters-in-the-industry will once again inform and enlighten. Details forthcoming…topics to include a discussion on how the industry reacted to COVID and the results of current research.
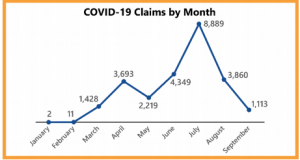
Sticking with workers’ comp, a Kimberly George/Mark Walls piece in National Underwriter noted TPA Sedgwick has handled:
45,000 COVID-19 workers’ compensation claims for their clients. 78% of those are closed with an average paid of $1050. 54% of the claims had no payments made.
That’s pretty consistent with findings from my firm’s June 25 survey of 35 payers and service providers (summary report download at no cost); from an interview back in June:
a lot of claims are filed with no payments…[a] respondent stated “96% of claims cost less than $3,500, but 4% are expensive.”
Finally, the news that Moderna’s vaccine will likely be approved for use this week is excellent news indeed. The company participated in Operation Warp Speed, the Trump Administration’s effort to jumpstart vaccine development by funneling $18 billion in taxpayer funds to organizations and companies working on vaccines.
One of the most positive signs is Moderna’s vaccine showed equal effectiveness among white and non-white subjects. As COVID has been particularly devastating in communities of color, this is critically important.
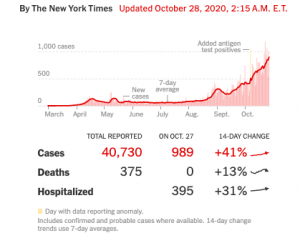
This from the NYTimes:
There was also no significant difference between its protection for men and women, or between healthy volunteers and those at risk of severe Covid-19 who had conditions like obesity and diabetes. For people 65 and older, the trial provided an estimated efficacy of 86.4 percent, lower than the overall estimate of 94.1 percent. But the apparent difference was not statistically significant.
So far, two potential differences between the vaccines have emerged from the F.D.A.’s reviews, but the findings may [emphasis added] reflect a shortage of data rather than genuine differences. The Pfizer-BioNTech trial showed that their vaccine started to protect against the coronavirus within about 10 days of the first dose. The trial of Moderna’s vaccine, by contrast, did not reveal such a striking effect after the first dose.
What does this mean for you?
Wear the mask and be very careful. This is very far from over.