Between doing grandfatherly duties (hanging out with our granddaughter), business obligations and snow plowing, it’s been a busy week.
here’s what’s up.
COVID stuff
Yeah, like you, I was hoping this pandemic would be just an unpleasant memory by now. Far from it.
Omicron has substituted transmissibility for lethality, so far more of us will catch COVID, but far fewer of us will get very sick or die. BUT – and it’s a huge BUT, the net impact is more of us are getting sicker.
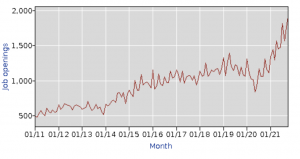
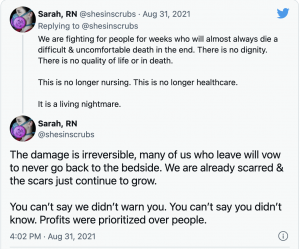
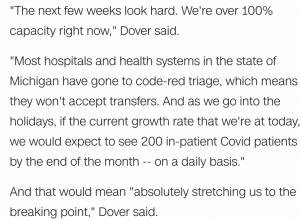
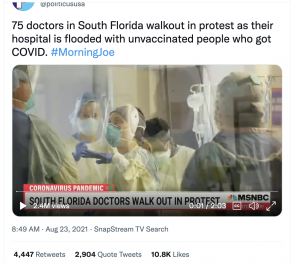
And the impact on healthcare facilities and the increasingly burnt-out people who work in those facilities is the worst it’s been since COVID arrived on our shores.
Another of those knock-on effects of COVID…hospitals can’t discharge patients because a) rehab facilities don’t have room, b) there aren’t enough home care providers to hep the patient recover at home. So, patients that COULD be discharged – thus freeing up beds for sicker people – aren’t.
Which leads to more stress on hospitals and hospital staff.
Side note – in case you missed it, the US has lost 10,000 ICU beds over the last year – because there aren’t enough healthcare workers to care for ICU patients.
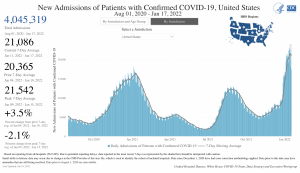
Last week saw a new peak in hospital admits for patients with COVID… most troubling is the rapid rise in kids 4 and under that have been admitted.
There’s been a lot of discussion about patients admitted with COVID vs patients admitted due to COVID. This needs unpacking.
Lots of us have health issues, which are called “morbidities”…asthma, high blood pressure, obesity, diabetes and the like. Very broadly, the more you have, the worse it is, because one exacerbates the other(s).
COVID is in that category...so while a patient may not have a bad case of Omicron, that patient’s immune system now has to deal with a respiratory (and perhaps other) problem(s) on top of being overweight, older, hypertensive and pre-diabetic. The result is the patient is in the hospital longer, takes longer to recover, and full recovery is less certain.
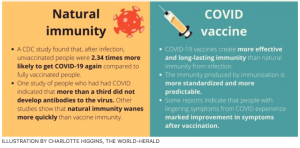
About those “co-morbidities”…some irresponsible media types butchered CDC Director Rochelle Wolensky MD’s comments on COVID and co-morbidities.
One such media type tweeted “CDC director admits over 75% of Covid deaths had at least 4 pathological conditions (comorbidities). Since the total death rate is 0.27% this means healthy people have a 0.0% death risk.”
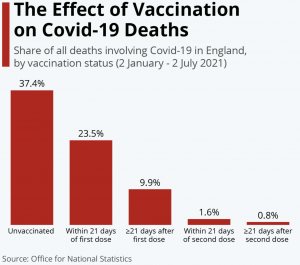
That is NOT what Dr Wolensky said. She was referring to COVID deaths among vaccinated individuals – NOT all COVID deaths.
Her point was that vaccinations protect us from COVID, but people in very poor health are still vulnerable; most of the vaccinated people who died were in very poor health BEFORE they got COVID.
Sheesh. This isn’t that hard people…
Education!
Registration for CWCI’s annual meeting is now open here; March 8 is the date. As of now it is live and will be streamed as well. Walnut Creek is the location, and attendees will hear solid research on the impact of COVID plus a study on injured worker access to care.
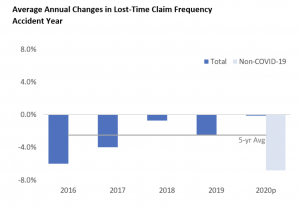
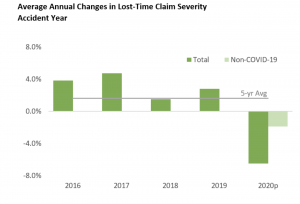
Today NCCI and several state regulators are discussing the impact of COVID – you can register for the webinar here. You can download the team’s report here.
Lots of great information. presented in an accessible format.
What does this mean for you?
Don’t retweet unless you check the actual source information, because you may look like an idiot.