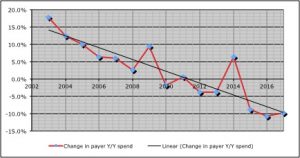
Work comp drug costs have dropped by over a billion dollars over the last eight years.
What’s even better news is this has been driven largely by sharply lower opioid utilization.
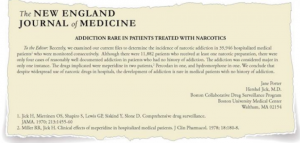
The bad news is there are still far too many patients suffering from Opioid Abuse Disorder brought on by massive overprescription of opioids.
Across all 29 workers’ comp payers surveyed by CompPharma, drug costs dropped almost 10 percent last year compared to 2016. (Total US drug costs decreased last year by 2.1 percent)

The results come from our annual Survey of Prescription Drug Management in Workers’ Comp, a project now in its fifteenth year.
Payers cited clinical programs as the primary driver of lower opioid and total drug spend. A key takeaway come from payers’ views of formularies:
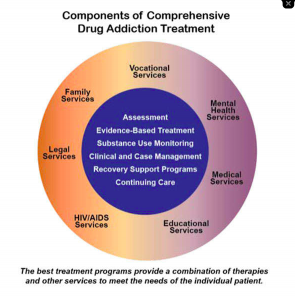
many respondents did NOT want to abandon their internal formularies in favor of a one-size-fits-all blanket formulary. These payers noted patients are all different, their needs evolve throughout the course of treatment and recovery, and therefore their pharmacy needs would change as well. While they were in favor of managed (state-mandated) formularies for initial fills, they want flexibility to adapt to the patient’s condition and needs without putting undue burden on the prescriber and pharmacy to comply with prior authorization requirements.
The public version of the Survey Report is available here for download; respondents received a more detailed version of the Report.
As the author of the Survey, I’d be remiss if I didn’t thank the respondents who have provided data and their views and opinions over the last 15 years. Their willingness to share their insights and perspectives has gone a long way to helping improve patient care.
I’d also note that work comp Pharmacy Benefit Managers have been largely responsible for reducing employer’s drug costs and opioid overuse. Another way to put this – PBMs have dramatically reduced their revenues by improving their customers’ and patients results.