It’s been a while since we dove into the latest research on COVID. Here’s a summary of where things stand.
“Cures”
Today there are no “cures” for COVID19. More accurately, no drugs or treatments have been proven to “cure” the disease.
A just-released study found that four drugs commonly used to treat hospitalized patients – anti-viral Remdesivir, hydroxychloroquine, Interferon, and Lopinavar:
“appeared to have little or no effect on hospitalized COVID-19, as indicated by overall mortality, initiation of ventilation and duration of hospital stay.”
The study was international in scope, used a randomized control format (a rigorous and well-regarded methodology), and enrolled over 11 thousand patients. Note the study has NOT yet been peer-reviewed
Gilead – manufacturer of remdesivir – disputed the study’s findings, which found:
no drug or combination reduced mortality, the chances that mechanical ventilation would be needed, or time spent in the hospital, compared with the patients without drug treatment. (NYTimes)
There are some indications that remdesivir may provide some benefit if administered early in an infection where it can tamp down the body’s immune response – which can be counter-productive.
Data
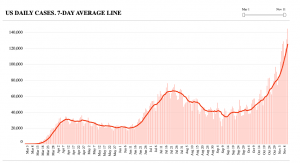
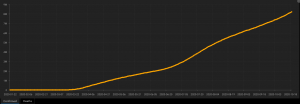
The US has administered over 119 million tests. About 8 million of us have been infected. And 210,000 have died.
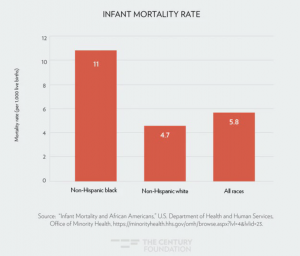
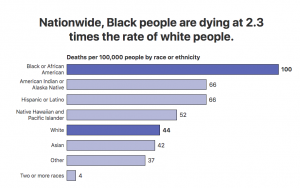
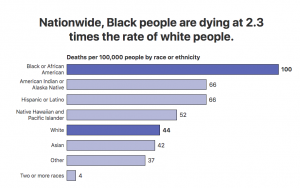
Black people are dying at more than twice the rate of White people. Other minorities are also dying at a far higher rate.
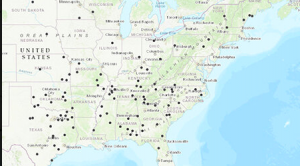
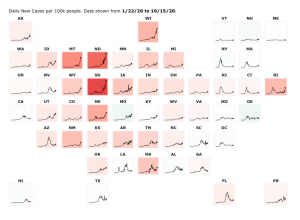
You can track infections, tests, and deaths in your state here.
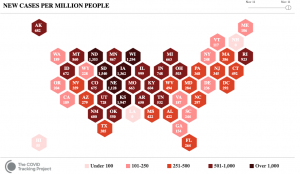
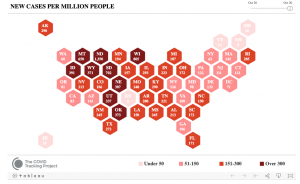
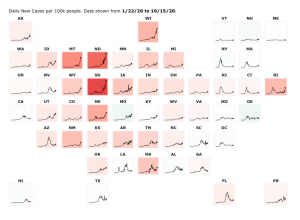
The infection rate is climbing – again – especially in the Dakotas, Montana, Nebraska, Wyoming, Rhode Island, and New Mexico. (the darker the color, the higher the infection rate)
Debunking the claim that COVID death rates are “inflated”
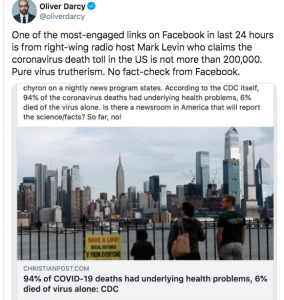
Some have claimed that COVID death rates are inflated as many folks that died of COVID had other major health conditions – COVID deniers have been spreading this lie in an attempt to downplay the disastrous effects of COVID.
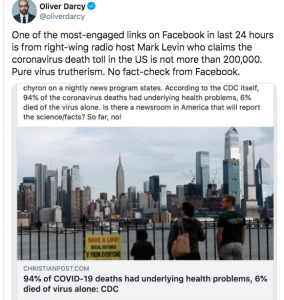
The CDC’s definition of the underlying cause of death is “the condition that began the chain of events that ultimately led to the person’s death.”
Think of it this way – if a person infected with COVID gets hit by a truck and killed, the cause of death will be listed as Motor Vehicle Accident – NOT COVID.
Similarly, if a person with COVID, hypertension and diabetes falls down the stairs and dies, the cause of death will be listed as “accidental fall”, NOT COVID
So, if a person with COVID, hypertension and diabetes dies after being admitted to the hospital, placed on a ventilator, given remdesivir, and administered oxygen dies, the cause of death will be listed as COVID.
What does this mean for you?
Wear a damn mask. Wash your hands.