This email arrived earlier this week;
I really enjoyed your newsletters until you started showing your political side; It’s unfortunate that you had to make that known to your audience.
I’ll leave aside the fact that I’ve been “showing my political side” for the more than two decades I’ve been writing MCM, moreover I’ve been transparent on my views on everything from:
- opioids to
- politics to
- physician dispensing to
- Congressional Republicans’ attacks on the ACA to
- Russia’s war on Ukraine to
- vaccination skeptics to
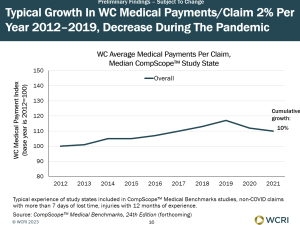
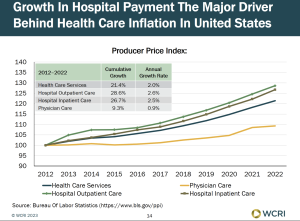
- the work comp industry’s failure to understand health care to
- TPA profiteering on managed care fees to
- some state legislators’ unconscionable failure to expand Medicaid to
- Texas’ legislators ridiculous grandstanding
- and about a gazillion other topics.
What is distressing about the former subscriber’s note is the underlying unwillingness to consider alternative viewpoints, to open one’s mind to different ways of thinking through issues, of critically evaluating one’s own beliefs.
That is especially true today, when we seem more willing to build walls than open windows.
I’d bet exactly none of my 2,510 subscribers agree with every one of my opinions and posts – nor should they. As I’ve publicly admitted, on occasion I’ve been wrong on facts, gone a bit too far or changed my opinion (right Rob Gelb?), mostly because a reader challenged me to think differently or I’d been lazy or lax in my research.
What’s distressing about the former subscriber’s note and subscription cancellation is it is symptomatic of a much broader “closing of the American mind.”
We lament society’s polarization while refusing to engage with others who may have different views.
We ostracize others for their views on a single subject, when we may well agree on most things.
We decry government’s ability to get anything done while supporting candidates who refuse to compromise.
I’m quite sure the unsubscriber and I agree on many things…perhaps the evil of Purdue Pharmaceuticals, the unconscionable profiteering of physicians dispensing drugs, the questionable ethics of non-transparent claims “fees”, the critical importance of getting patients to the right provider quickly, the problems with brokers and consultants who follow the latest fad instead of doing the hard work to actually help their employer clients (nurse triage, anyone??).
Alas we’ve become latter day Inquisitors, willing to demonize anyone that doesn’t agree entirely with us. The Pope’s inquisitors tortured, burned, and crippled Cathars for the sin of their different interpretation of Catholicism.
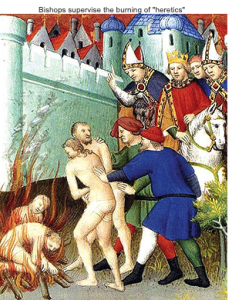
Today, nine centuries on, we are at risk of returning (hopefully only metaphorically) to the horrific days of the 1300s.
What does this mean for you?
We are far more alike than we are different, share far more similarities than differences.
Let’s try.