We are finishing up our Annual Survey of Pharmacy Benefit Management in Workers’ Comp…here’s three findings from the 15+ we’ve done so far.
1) 60% of respondents are reporting an increase in overall drug spend – with reasons varying from more claims to an uptick in catastrophic cases to jurisdictional impacts.
While we’re a long way from done and more respondent data is coming in, if the trend continues this would be the second year of “non-decrease” in spend, signaling that the years-long drop in spend has stopped – and may have reversed.
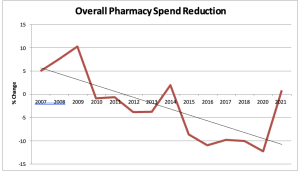
This from last year’s Survey…this year’s will include 2022 and 2023 data.
3) Most respondents see a future for AI in the PBM world… but the emphasis is definitely on the future. There seems to be significant hesitation around implementing AI-based tools at this point. Ultimately, respondents see a range of “futures” – ranging from 100% automation of the entire process driven by AI to those who see AI focusing largely on early trend identification and clinical management improvements.
If you woulds like to participate, leave your info in the comment box below.
Public versions of our Annual Survey report are available for download here at no cost and no registration – note respondents get a much more detailed version of the report.
Thanks to HSA’s Jay Stith and Helen Knight of CompPharma for their work on this year’s Survey.


