It sure looks like they/you have.
WCRI’s latest report finds:
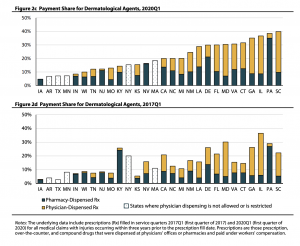
- Physician-dispensed drugs (PDDs) accounted for more than half of drug costs per claim in Q1 2020 in four states – Florida, Georgia, Illinois, and Maryland.
- In 12 states, doc-dispensed dermatological agents accounted for most payments for this drug class.
- Louisiana is worst-off, with employers paying $190 per claim for dermo drugs in the 1st quarter of 2020…Illinois is right behind at $181.
- Kansas and Connecticut saw payments for those dermo drugs triple from Q1 2017 to Q1 2020.
That profit-sucking prescribing by docs in Connecticut is why total drug spend increased 30% in the Nutmeg State – making it one of two states that had drug spend increases. Florida – the home state of PDD – was the other. (Across all subject states, drug costs dropped 41%.)
Having lived in CT for over 20 years, I’m really stumped by the precipitous increase in skin care drugs.
What could POSSIBLY be driving this massive need for occupationally-driven skin care/topicals?
Did sun spots create a pandemic of skin cancer but somehow only affect the second-smallest state?
Did a massive refinery accident expose tens of thousands of workers to burns or skin infections?
Did a hyper-virulent new breed of poison ivy run rampant, affecting thousands of landscaping and municipal workers?
Did the emerging cannabis industry fail to protect its workers from fertilizer burns, exposing thousands of workers to painful blisters?
Did everyone in Connecticut suddenly become unable to swallow a pill?
Of course not.
The real question is this:
why haven’t insurers, TPAs, and self-insured employers used CT’s Medical Care Plan to ban physician dispensing? Payers including the Workers’ Comp Trust of CT have pretty much eliminated physician dispensing.
It’s not just Connecticut. PDD costs are outrageous, and all credible research indicates PDD is totally unnecessary, increases medical costs, and prolongs disability.
WCRI’s research should be a call to action. Legislators, regulators, and payers are doing their policyholders and clients a disservice by failing to aggressively attack physician dispensing.
And those clients and policyholders are equally at fault – it is up to you to work with your PBM and payer to stop this rampant profiteering.
What does this mean for you?
Yeah, I know it’s hard. Most important things are. Get to it.



Great article Joe, as usual. The findings do not surprise me at all. In my experience, most of the PBMs are doing something to try to combat this, some in aggressive ways especially as it relates to formulary management and many of these drugs requiring approval before being paid. The issue is twofold, one is that all of these drugs are handled retrospectively meaning they are already dispensed by the doc without any type of pre authorization via the payer/PBM. This presents a huge issue when the payer denies payment for things like clinical appropriateness because the physician dispense companies simply go after the payer aggressively for payment. Second, when the adjusters receive threatening calls to make payment, they typically go ahead and pay anyway. If you look at total PBM and payer data history you will find a consistent theme across the industry where there are physician dispensing denials via the PBM only to find the payer issuing payment anyway behind the scenes. The PBMs have in my opinion been left with trying to resolve this challenge, only to have the payers turn around and issue payment anyway. If you are a savvy PBM you should know this is happening and be partnering with your clients to get creative with a more thorough end to end solution. Of course, I also believe the States are not doing enough to resolve this issue either.
PBM Anon – we agree. Payers must work WITH their PBMs to attack PDD, not shortcut their efforts.
Payers need to hold claims staff accountable as well. To quote the estimable Ms Reagan…”Just Say No”.
and stick to it.
be well – Joe
Joe Great topic and a tough one. We have engaged the states to assist as well with little support. As you say a tough challenge that we payer, employer pbm and regulatory partnership to win!
agree Mike – all parties need to work together. Made a lot of progress years ago but that has slipped away.
Employers and insurers need to hold docs accountable and use MCO/MCA regulations to ban PDD.
Tough for PBMs to manage clinical issues with these dispensing docs prescribing anything they want.
be well – Joe
Hi Joe,
Here in California we went through some challenging times dealing with bills for compound topical preparations generally prescribed for pain. These were rarely authorized by utilization review and were most often ordered by physicians from a fixed menu- not individually compounded to meet specific patient needs. In addition, while the ingredients were purchased in bulk, they were billed to carriers at the highest per unit cost to maximize profits. We have learned that the formulas themselves were often derived from the price lists with no regard for potential interactions/toxicity.
Hello Lynne – and thanks for the note. unfortunately WC is seen as a piggybank by unscrupulous “providers” interested in nothing other than cash.
Keep fighting the good fight.
be well Joe