myMatrixx’ Drug Trends Report is out – here are my key takeaways.
Behavioral Health
Kudos to the authors for the comprehensively addressing behavioral health (BH) issues. Among the takeaways are:
- Not addressing the mental health of injured workers can delay return-to-work, increase the risk of opioid addiction or both.
- Although mental health conditions rarely can be proven as work-related on their own, they often arise as a result of work-related injuries. (italics added)
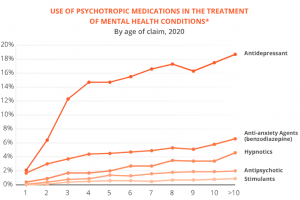
- The older the claim, the more likely psychotropic medications were prescribed.
What this means
Claim closure and settlement are driven by the recovery of the patient. You are not going to get those claims closed or settled unless and until BH issues are resolved.
Opioids and benzos drive claim outcomes
The Report referenced a 2014 JOEM study noting the more dangerous drugs a patient is prescribed, the higher the claim cost – and the longer the claim is open.

While there’s certainly a severity issue at play here, the central takeaway is minimizing the inappropriate use of short- and long-acting opioids and benzodiazepines is key to patient recovery.
What this means
If your PBM and clinical staff aren’t on top of opioids and benzos – as in instantly aware of scripts and able to deploy clinical support expertise – those patients are far less likely to recover – and you’re going to pay dearly.
Both of these issues – behavioral health and dangerous drugs – are critically important to patient recovery and claim closure.
As I noted yesterday, far too often WC payers choose vendors/partners based on the wrong criteria.
Nowhere is this more common than for pharmacy management. Price is important, and service is key – but both are secondary to the impact of pharmacy on claim outcomes.
What this means for you.
More than any other service, PBMs drive claim outcomes – for better or worse.
note – myMatrixx is an HSA consulting client. I’m honored to work with them.


