Three key takeaways from this week’s COVID19 news.
Do we KNOW how bad things are, who’s dying, and Remdesivir.
- Do we know how many are infected, the death rate, and the number hospitalized/in the ICU/on ventilators?
No.
We are three plus months into the crisis and if anything, the picture is muddier than it was a month ago. From the highly-credible COVID Tracking Project;
it is impossible to assemble anything resembling the real statistics for hospitalizations, ICU admissions, or ventilator usage across the United States.
Also from the Project:
the CDC does offer a national-level account of “specimens tested,” this data is incomplete and lagging, and it uses a different unit (specimens tested) for total tests than for positive results (which are counted in people). This makes it impossible to accurately match testing totals with positive tests to infer a complete picture of COVID-19 testing, even at the national level…a simple count of identified COVID-19 cases doesn’t show the true location or comparative severity of outbreaks. Simple case counts show where people are being tested, not where people are sick. [emphasis added]
Yep, the greatest country on Earth can’t even capture and accurately report infections, hospitalizations, and deaths…you should be pounding your head against the wall.
Or maybe just scream in frustration…
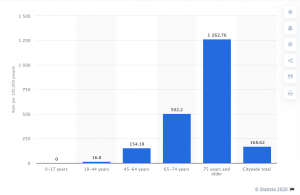
2. Who’s dying.
In the New York City, it’s mostly older folks.
From Statista…
Alas, our nation’s leaders still do NOT KNOW how many of our loved ones in nursing homes have been killed by COVID19.
Almost three weeks after CMS Administrator Seema Verna took to the podium to announce HHS would begin publishing the numbers, we’ve seen nothing.
3. Finally, Remdesivir is NOT a cure – far from it.
The results of a study conducted by NIAID on about 1,000 patients found it does shorten the course of COVID19 – by four (4) days – in some patients. Manufacturer Gilead hasn’t said what remdesivir will cost, but indications are about $4,000 per patient.
NIAID’s study found the anti-viral drug:
- has been shown to be safe in humans,
- is given intravenously (it is injected into the blood stream),
- the course of treatment is 5 – 10 days,
- has to be administered in a hospital, and
- the vast majority of patients who recover at home will NOT get the drug.
Perhaps the most important impact will be shortening the course of COVID19 (although that didn’t happen in all patients who got the drug). This will free up more bed-days in facilities and allow them to treat more patients.
Note an earlier study in China did not find remdesivir was effective in treating COVID19. From the study: “Remdesivir use was not associated with a difference in time to clinical improvement”
Lastly, who will actually get the drug depends on luck – some hospitals will get it, others will not, with no rhyme or reason.
For my work comp readers, over at Workers’ Comp Insider Tom Lynch has a quick summary of COVID19 and its impact on workers’ comp.
What does this mean for you?
We should expect way more from our elected officials.


