We’ve just about completed the 16th (!!) Survey of Prescription Drug Management in Workers’ Comp, and there are two key findings you need to know.
First – total opioid spend in 2018 dropped 23.2% across all 27 respondents (ranging from very large TPAs to state funds to insurers to small state-specific payers). The average decrease among respondents was just over 22%.
That dramatic reduction comes on the heels of a 16% reduction from 2016 to 2017, and a 13% decrease in 2016.
From last year’s Survey; each numbered column denotes a respondent’s results (2019 Report will be out in August)
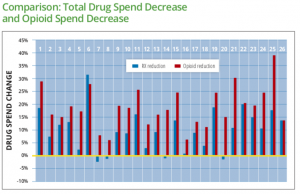
Over the last few years, payers and PBMs have cut the amount of opioids dispensed to work comp patients by more than half.
While cost reductions are good news for employers and taxpayers, when you talk with payers its mostly about patient safety and return to functionality. Patients taking opioids over long periods aren’t getting better, aren’t going back to work, and most (but not all) are not functioning very well. That means they aren’t the parents, friends, daughters or sons, grandmothers or grandfathers they can or want to be.
Second takeaway: payers are anything but satisfied or complacent. All the 27 people I’ve talked with to date remain focused, committed, and completely engaged in continuing to fight the good fight against overuse of opioids. They’ve asked me what other payers are doing, what they can do differently, what works and what doesn’t.
That’s a great relief. One would understand if payers’ focus was shifting to other issues, now that they’re seeing massive progress in the battle over opioid over-prescribing.
With some exceptions, the knottiest problem remains how to help chronic opioid patients find other ways to handle their pain, to help them function at a higher level even with chronic pain. Payers are very creative and dedicate lots of dollars and time to solving chronic opioid usage. This focus will continue to help patients get better, while reducing costs for employers and taxpayers.
I’d be remiss if I didn’t note – once again – that work comp is leading the rest of the world on solving the opioid issue. You knew about it sooner, took drastic action much faster, and are delivering much better results than Medicaid, group health, or Medicare.
Yeah, the workers’ comp industry is often maligned for its many faults and challenges. But this is one area – and a damn important one – where you’ve got much to be proud of.
What does this mean for you?
Well done. Stay focused.


