CompPharma’s latest Survey of Prescription Drug Management in Workers’ Compensation (past reports available for download) has some very welcome news; over the last two years, opioid spend is down by one-third.
Most of that reduction is from improvements in clinical management and changes in prescribing patterns and behavior.
(I’m finishing up this year’s report draft tomorrow…)
Of the 28 respondents to this year’s Survey, 25 had double-digit decreases in annual opioid spend, and six saw drops greater than 25%.
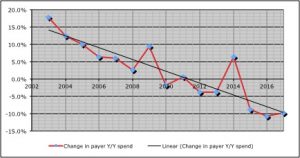
The opioid spend reduction was a big driver of a reduction of 9.8% in total drug costs across all respondents – the sixth decrease over the last 8 years.
Couple early takeaways:
- A dozen respondents cited improved/upgraded/expanded clinical management programs as key drivers of the change.
- Big decreases in compound drug costs were also noted by several respondents, with most seeing reductions greater than 30%.
- In response to the question “Where do prescription drug issues rank compared to other medical service issues at your organization?,” drug costs were rated as a 4.1 on a 5 point scale, (more important than other medical service issues).
This last is telling.
After dramatic improvements in opioid utilization, respondents remain quite concerned about the impact of drugs on claim closure, disability duration, and patient safety.
What does this mean for you?
Progress is great, and much remains to be done.


