is hospitals hoovering dollars out of employers, work comp insurers, and taxpayers’ wallets.
WCRI’s latest research report on hospital costs is a must-read for anyone involved in work comp claims, medical management and actuarial issues. Kudos to Drs Olesya Fomenko and Rebecca Yang for their excellent work.
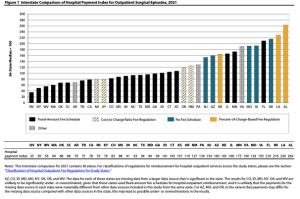
The study focuses mostly on how payments for outpatient surgery vary across the different types of fee schedules (no fee schedule vs fixed amount vs cost to charge ratio vs percent of charges…)…and how those payments have changed over time.
But there are several other issues that I’d argue are more impactful.
- It’s not so much the type of fee schedule as other factors…
- there’s a LOT of variation between states with the same type of FS
- failing to expand Medicaid is a big problem for hospitals
- Basing fee schedules on percent of charges is a really bad idea…
- states with %-of-charges FS had – by FAR – the highest costs, averaging more than 3 times what Medicare pays. (Medicare reimbursement is slightly above break-even for hospitals)
- `hospitals easily game the “fee schedule” by jacking up list prices
- 2 of the three states with the largest increases in hospital payments had FS based on %-of-charges
- States with NO fee schedules were not quite as bad – averaging “only” 225% of Medicare
- Clearly network arrangements have failed miserably.
What does this mean for you?
Actuaries…check the inflation trend to predict where costs will be in the future
Medical management folks…dig into your data to identify the worst offenders, and direct care AWAY from them. Hint – HCA facilities are usually among the worse offenders.
Bill reviewers – STOP relying on network discounts and start getting LOT smarter about dealing with facilities.
