The reaction to yesterday’s news that pharmacy costs have dropped by over a billion dollars was a bit disappointing – and missed the key takeaway.
That is – we’ve made a ton of progress, and we still have a long way to go.
Instead, some asked “where are the savings going?”, claiming employers and patients aren’t benefiting from the reduced cost.
A Kansas legislator was among those positing that question; perhaps he was unaware that Kansas employer’s premiums dropped 7.6% this year. Kansas’ results mirrored the nation’s and other states:
- California’s rates are down 22% over the last four years.
- New York is looking at an 11.7% cut on top of last year’s 4.5% decrease.
- Maine employers will see a cut as well due to a loss cost decrease of 12%.
Of course, there are many other reasons rates and premiums are dropping across the board:
- a nine-year long economic expansion;
- a solid job market;
- continued decline in claim frequency and anecdotal reports of a drop in total claim counts;
- better control of medical costs; and
- lots of capacity in the insurance market
are the most significant contributors.
Another critic complained that “the savings are going into insurers’ pockets.” There is some truth to that, as workers’ comp insurer profits remain at near-record levels despite the continued decrease in premiums.
(Re increased benefits for patients, that is a state regulatory issue as indemnity benefits are almost all driven by a formula involving cost-of-living benchmarks)
But the key point is this – work comp has done great work eliminating opioids – and that is wonderful news by any standard.
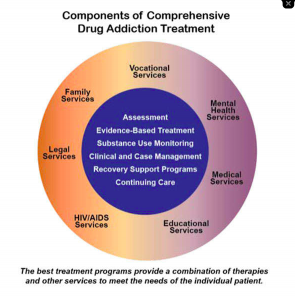
As CompPharma’s report details, a key driver of the drop in drug costs is lower opioid utilization. That is very good news indeed; fewer patients are getting opioids, and other reports indicate dosages and treatment duration are declining as well. Moreover, the drop in opioid usage in work comp is far greater than the overall decline in drug spend, indicating we are doing a far better job than the rest of the insurance world despite the difficulties inherent in managing drug utilization in comp (no economic levers to influence consumer behavior, few states with pharmacy network direction, widely varying regulatory environments).
For fifteen years I’ve been interviewing the people most responsible for addressing the opioid crisis in work comp. While costs are important, without exception these professionals see their job as improving patient care, reducing the risks and dangers inherent in opioid prescribing, and helping patients recover quickly.
Their relentless focus is leading to healthier patients and lower costs for employers.
We have a very long way to go. While lots of work from lots of people has helped dramatically reduce the initial (or even more problematic second) opioid script, the much tougher challenge is helping long-term opioid patients reduce and end their use of the drug.
Some payers are making solid progress; you can hear from four of them at IAIABC’s annual meeting this fall. I’ll be moderating an intensive review of how these payers are successfully helping patients reduce opioid consumption and get back to being themselves.
What does this mean for you?
Congratulations on making major differences in many patients’ lives. Now the hard work begins.