A nurse was convicted of “reckless homicide and impaired adult abuse” after she inadvertently – and unintentionally – injected a patient with the wrong drug. RaDonda Vaught faces six years in prison
I’m pretty angry about this – and that anger is NOT directed at Ms Vaught, but rather at a grandstanding prosecutor, a negligent hospital, and a healthcare delivery system that is far less than honest with its workers and patients.
The death occurred when Ms Vaught gave Ms Murphey vecuronium instead of Versed. Sources tell me that vecuronium (a medication used as part of general anesthesia to provide skeletal muscle relaxation during surgery) is a significantly more powerful relaxant than Versed (a benzodiazepine, similar to Valium).
Okay, here’s the reality.
- Medications are accessed via a secure cabinet which requires multiple steps to dispense a drug. Omnicell – the cabinet used by Vanderbilt did not have some controls that would – in all likelihood – have prevented the error.
- There’s no question Vaught overrode system controls – but she did so because she did not know that the drug prescribed – Versed – was only available in the generic form – midazolam – from the Omnicell cabinet. Vaught also did not know that midazolam was the generic form of Versed.
- Instead Vaught typed “Ve” in the cabinet’s search function – and the cabinet’s electronic system responded with vecuronium. Vaught then selected vecuronium and administered it to Murphey.
- The prosecutor said Vaught’s decision to override the control was central to obtaining an indictment.
In fact thousands of nurses do this – override an automated dispensing cabinet’s built-in controls – hundreds of thousands of times every year. Vaught is one of thousands who have to make decisions when the doctor’s orders aren’t easily followed – or followed to the letter. Instead they have to use their judgment.
From the Institute for Safe Medication Practices:
The hospital where RaDonda worked allowed nurses to remove certain medications via override, and it is highly likely that, prior to this event, midazolam and vecuronium had been removed from an ADC via override in this hospital. Also, it is unlikely that nurses, including RaDonda, perceived a significant or unjustifiable risk with obtaining medications via override. In fact, removing certain medications from an ADC via override is an accepted risk in healthcare and one that many practitioners take to provide care to their patients. [emphasis added]
Vaught reported the error – as is common practice – with the understanding that doing so would not result in legal action against her.
Again the ISMP:
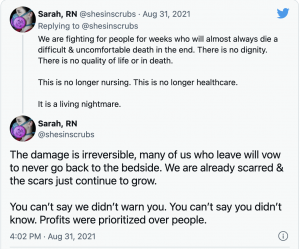
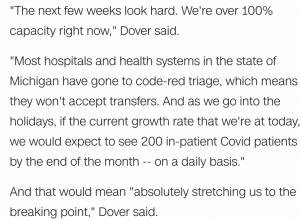
Criminal prosecution has worrisome implications for safety. It can inhibit error reporting, contribute to a culture of blame, undermine the creation of a culture of safety, accelerate the exodus of practitioners from clinical practice, exacerbate the shortage of healthcare providers, perpetuate the myth that perfect performance is achievable, and impede system improvements.11 [emphasis added]
Vanderbilt University Medical Center selected and installed and trained staff on the Omnicell cabinet – a decision that was directly responsible for Murphey’s death. From KHN:
A lead investigator in the criminal case against former Tennessee nurse RaDonda Vaught testified Wednesday that state investigators found Vanderbilt University Medical Center had a “heavy burden of responsibility” for a grievous drug error that killed a patient in 2017, but pursued penalties and criminal charges only against the nurse and not the hospital itself
Vanderbilt took several actions that resulted in the medication error not being disclosed to the government or the public, according to county, state, and federal records related to the death. Vanderbilt did not report the error to state or federal regulators as required by law, a federal investigation report states. The hospital told the local medical examiner’s office that Murphey died of “natural” causes, with no mention of vecuronium,
Reality is Vanderbilt avoided criminal responsibility and Vaught gets the blame.
If you object to this, please sign a petition to ask the court to grant RaDonda clemency. (Thanks SW for the head’s up)
From Hospital Watchdog

Finally, there’s this.
Prosecutor Brittani Flatt’s closing argument included this reprehensible statement:
“RaDonda Vaught probably did not intend to kill Ms. Murphey, but she made a knowing choice,” [emphasis added]
What absolutely ignorant and inflammatory bullshit.
Flatt’s statement implied that Vaught might have intended to kill Charlene Murphey, a statement that has no basis in fact, was completely contradicted by everyone involved, and is incredibly insulting to Vaught. Flatt should disciplined for her egregious statement.
Moreover, there’s no evidence Vaught made a “knowing choice”, in fact just the opposite – unless the “knowing choice” she made was to circumvent controls built into the drug cabinet, a “choice” she and thousands of her fellow nurses make every day.
What does this mean for you?
Medical professionals will be a LOT less likely to report errors.
Another clear sign that our health care system needs major overhaul.
Don’t go to Vanderbilt University Medical Center.
reminder – tomorrow is April First.




 Why?
Why?