Even when dealing with the same health system it is important to monitor the facilities you are directing care to.
In parts 1 and 2 of this series, we looked at two Florida facilities and showed the complete lack of correlation between the facility’s cost and the quality output.
Today, we look at three facilities ALL IN THE SAME HEALTH SYSTEM… IN THE SAME CITY… with differing costs and outputs.
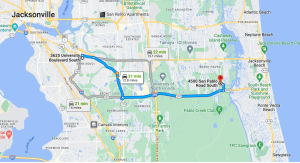
Three HCA facilities: HCA Houston Healthcare Medical Center, HCA Houston Healthcare West, and HCA Houston Healthcare Northwest – all within 40 minutes of each other.
Based on data from Health Strategy Associate’s Facility Assessment Tool, HCA Houston Healthcare Medical Center is superior across the board when compared to HCA Houston Healthcare Northwest and equal to or better than HCA Houston Healthcare West.
Versus West and Northwest, the clinical outcomes from HCA Houston Healthcare Medical Center are more than 2x the other two. The patients… AKA your clients… are more than 2x as content with HCA Houston Healthcare Medical Center and you/your boss/your board/your shareholders will be too when you pay less for higher quality care.

Again, higher quality facility at a lower price.
Shop Around! This dynamic occurs all over the country – check your utilization and your network to make sure you know just what facilities you are using.