The most popular formula for calculating the “value” of healthcare is pretty simple…
If you want to get a bit deeper into details, there’s this…
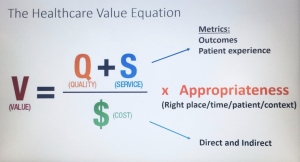
It’s about the “quality” of the medical procedure (was it done right? was the patient re-admitted? was there a surgical error or infection), perhaps the appropriateness of that procedure, and the “patient experience” – measured…somehow.
Pretty much every formula, discussion, or description of the healthcare value equation is focused on “outcomes” defined as the result of a surgery or treatment (did the patient get better?) or avoidance of sickness or injury (did the patient stay “healthy”).
None – as in none – focus on what’s really important to you and me –
Did the healthcare we received maintain/improve our ability to function – to raise our kids, work, exercise, function in society, do things we like to/have to do.
Functionality is the only “value” metric that matters, yet pretty much no one in healthcare and no healthcare organization – except in workers’ comp – talks about functionality, measures their results based on functionality, reports member functionality, studies it or seeks to improve overall member functionality as a core goal (except for a few unique healthplans).
Further, employers, who pay hundreds of billions of dollars on healthcare insurance premiums don’t even think about the impact of that healthcare on employee functionality/productivity.
Why?
Procurement, CFOs, finance departments and management are constantly challenged to show a return on investment on any project, hire, new initiative, acquisition or investment.
But never when they are buying healthcare – which, after payroll, is the biggest single part of the budget for most service companies and a major cost for every type of employer – public, private, not-for-profit.
Nope, it’s the thickness of the provider directory, whether or not some health system is in that directory, perhaps some “quality” rating, plus the biggie – cost.
What does this mean for you?
We are buying healthcare all wrong.



Amen, brother. A couple of years ago, a position paper with recommendations for the use of “functional metrics” to gauge the progress and effectiveness of medical treatment was jointly published by the American College of Occupational & Environmental Medicine, in collaboration with the American Psychological Association and NIOSH. Here’s a link to that paper: https://acoem.org/Guidance-and-Position-Statements/Joint-Statements-Summit-Recommendations-Proceedings/Recommendations-from-the-2019-Symposium-on-Including-Functional-Status-Measurement-in-Standard-Patie
Thanks Jen – Excellent resource for metrics and recommendations.
be well Joe
Right on the money again Joe. But, as the consummate advocate for rehabilitation (PT/OT) providers I will say it is the only outcome that matters. We have been measuring ourselves and outcomes by function for a long time. Yes, pain as well but function is the most important outcome. This is not only with our injured workers but all patients. Most of the quality improvement measures for therapists as determined by CMS are based on function. CMS is also bonusing (or penalizing) providers for participation in their MIPS (Merit-Based Incentive Payment System).
Thanks for the note and observations Mark, as well as the discussion of CMS’ MIPS.
I’m not aware of inclusion of mental health metrics in these standards/objectives but I have only a cursory understanding of MIPS’ metrics and methodology. Given our increasing understanding of hte importance of mental health I’d suggest it should be included in evaluating functionality.
be well Joe