We are getting more data on what insurers pay for COVID treatment, data that will help business folks better plan for the future.
AHIP’s June analysis provides a range of estimates based on different infection rates; the chart below reflects an assumed infection rate of 20%. (the methodology and database are robust and pretty complete, see appendices for details)
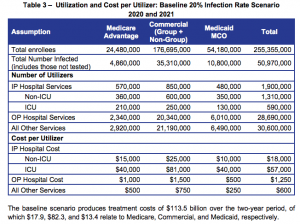
Note the “cost per utilizer” data which indicate average commercial insurance costs of:
- $25,000 per non-ICU hospital admission
- $81,000 per ICU hospital admission
- $1,500 per outpatient hospital admission
- $750 for all other medical treatment costs
Patient cost-sharing could add another 8% or so to total costs, however as most insurers have waived cost-sharing requirements, in most cases that 8% would be added to insurers’ costs.
There are other sources for cost estimations including FAIR Health and the Kaiser Family Foundation. An extensive discussion of their methodologies is here, KFF uses pneumonia with significant complications as a proxy for COVID19, while FAIR Health’s numbers are based on actual COVID19 treatment costs. (I discussed FAIR Health’s findings in depth back in July.)
Other research is here.
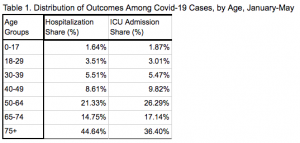
For those interested in the percentage of those infected who are hospitalized, a chart from the above link is below.
Costs for treatment of workers’ comp patients may well be higher, however this will vary greatly depending on the state, fee schedule limits (if there is a fee schedule) and network arrangements.
What does this mean for you?
All available data indicates medical treatment for COVID is not that costly. Yes there are some cases that require long-term, extensive ICU care with ventilator assistance, but they are relatively few.


