The average California MSA includes almost $49,000 for drugs – about half of all future medical expenses.
69% of MSAs included funding for opioids.
But when researchers compared the MSAs to a
“case-matched control group of closed workers’ comp permanent disability claims for similar injuries, the authors found that the WCMSAs called for much stronger opioids, as average cumulative morphine milligram equivalents (MMEs) allocated to WCMSAs with opioids were 45 times the level used in the control group during the life of the claim.” [emphasis added]
Why?
Especially when the report goes on to say:
Federally mandated formulae to financially account for decades of sustained individual opioid use are at direct odds with a growing body of clinical evidence — and a widespread recognition — that opioids are often over-prescribed for the management of chronic, non-cancer pain.
The Feds want/require employers and insurers to pay for another 20 years of opioids, at relatively high doses, for claims that should not be getting opioids.
This is what makes all of us nuts; one hand of the government is pushing us to assertively reduce opioid use, while the other hand demands we pay for opioids for another two decades.
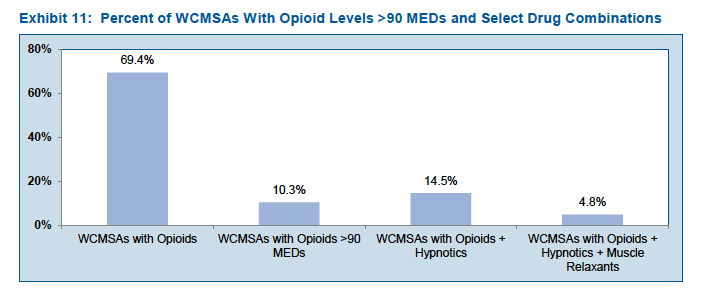
Worse still, many of the MSA patients are also taking hypnotics and/or muscle relaxants.
[chart courtesy CWCI]
A couple thoughts…
The claims with MSAs may well be those that payers can’t resolve, where the patient, their attorney, or their provider just won’t cooperate in efforts to reduce opioid use. Thus, the MSA projections make sense.
Why are these patients being prescribed – and ostensibly consuming – a high volume of opioids for an extended time when clinical guidelines and best practice clearly contradict this practice, and other patients with similar conditions aren’t getting these drugs?
What does this mean for you?
We are making progress, but we have a very long way to go – and CMS isn’t helping.



Many jurisdictions in WC give authority to the treating physician, and many do not want to wean their patient from these prescriptions, even when nurses or Peer physicians bring it to their attention, as the employee is receiving many times what is recommended. Most WC statutes and Judges support the treating Physician.. so moving the employee to another Physician (if you can find one to take the case).. is difficult or impossible. We need assistance from the individual states to take a look at these situations.. and add something in the statute to assist in these type of scenarios.
64,000 drug overdose deaths in USA (Jan 2016-Jan 2017)….fentanyl and synthetic opioid deaths doubled in 1 short year! WSJ 12/27/2017.
This is one of the main reasons for the move to Evidence Based MSA (based on Qualitative and Quantitative Medical Standards of Care). CMS’ requirement that MSAs cover medications for Life Expectancy is not based upon any semblance of a Medical Standard. This CMS Guide is used to artificially inflate the allocation’s cost. Requiring RREs to fund Opioids for decades is criminal.
In studying live claims data, a few themes arise: 1) Claims which are poorly managed present with higher Rx costs 2) Prescription drug use decreases over time and 3) changes with advancing age. When comparing against MSAs there is misalignment in the Part D forecasts, significant enough to warrant a change in guidelines for calculating Rx use. We are actively quantifying this issue for the release of an upcoming white paper which will add value to this discussion.