Back claims account for around a quarter of all workers’ comp claims. They are also among the toughest to handle; what appears to be a simple strain at first report may end up a long-term, permanent disability claim.
Three recent studies on back pain, the treatment thereof, and how treatment varies from place to place are well worth your consideration.
Here’s the quick summary of each – followed by what it means for work comp patients, providers, and payers.
First up, a comprehensive study of management of nonspecific back pain treatment options will begin shortly, funded by the Patient-Centered Outcomes Research Institute (PCORI).
The Comparison of Surgical and Nonsurgical Options for Management of Chronic Nonspecific Low Back Pain will assess outcomes for patients receiving surgery (lumbar fusion) vs non-surgical treatment. This is a randomized control trial, so the results will be instructive indeed for work comp regulators, payers, and providers.
HOWEVER, a decade ago a very similar study was conducted which indicated similar outcomes for surgical and non-surgical patients – but this result was not deemed conclusive because lots of patients who were put in the “surgery” group chose not to have surgery and vice versa.
Implications for work comp – a valid study will greatly help regulators determine the approval process and standards for back surgery.
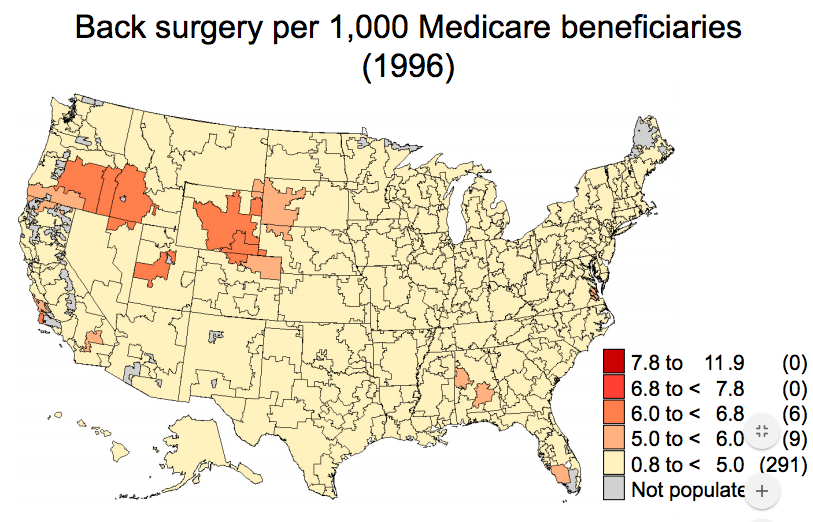
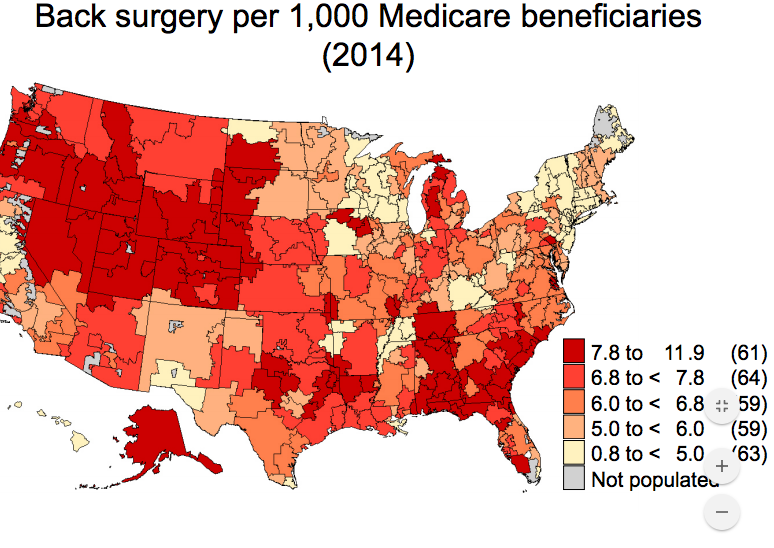
Whether or not you get back surgery appears to depend more on where you live than what your symptoms are. That’s the conclusion from a recent Dartmouth analysis of Medicare data. The other major takeaway – – despite the lack of credible evidence that surgery produces better outcomes.
maps below are from Dartmouth Diffusion project.
Notice how surgery rates didn’t move much at all in New England, but dramatically increased in the southeast and Rocky Mountain regions.
If you want to know why, there’s this from the NYTimes article: “physician beliefs about the benefits of surgery were associated with surgical variations.”
Implications for work comp – Regulators, use NATIONAL guidelines, and don’t rely on local providers to drive your guideline selection.
Supporting this research is this – drugs don’t seem to help resolve back pain any quicker. A guideline was just released by the American College of Physicians advocating non-pharmaceutical approaches for treatment of back pain.
Implications for work comp – I’d be repeating myself…



How are the maps of the US broken up? Something similar to counties?
Medicare discharge regions
There is a great book about back the placebo effect of surgery called: Surgey: The Ultimate Placebo.
You should check it out.
Written by an orthopedic surgeon.
A “stakeholder consensus” study of a condition that does not exist, “nonspecific low back pain”, will not be valuable, just as a consensus study of nonspecific cancer treatments would produce only confusion. Cancer is many problem, each needing specific treatments. Low back pain is cause by a large family of problem; at least 50 are reasonably common. Shaking them in a bag, calling them all the same thing, and randomizing a single treatment is nonsense. May I borrow a phrase, call it Fake Science? Hundreds of millions of government spent! Any study that does not start with a proper diagnosis of each case of back pain is doomed; one size does not fit all. Warning: good diagnosis cannot be accomplished with imaging alone. Clearly, we have WAY too much surgery. Try correlating back surgery and disability rates, as a nice quick start, then use the results to justify the need for a skilled clinician non-surgeon to authorize every surgery. That will get you more than half the way to where you want to be. To get the good diagnoses and outcomes, you must reimbursements the good diagnosis people more and the surgical people less. You do get what you pay for, and we are paying for a lot of surgery, without any financial relationship to outcome. This is health plan design and finance, not medicine.
Hello George – thanks for the comment. Couple observations.
Certainly agree with many of your points, especially the consequences of Fee For Service (FFS).
I disagree with your characterization of the project. In fact, diagnosis is part and parcel of the study. As you will note in the link provided to PCORI’s Funding Announcement, the research specifically calls for research on diagnosis. Moreover, the project solicits submissions that will define the research methodology and focus – PCORI reviews the researchers’ submissions – PCORI does not design the studies, it selects ones that best meet the objectives.
Joe, Great, I’ll spread the word. g
Thanks for the update, Joe. The new randomized trial will be helpful; maybe we can definitively put over-treatment behind us. Or maybe we’ll be surprised and find out something unexpected. Either way, it will be good to know.