Headed out on a much-needed vacation; MCM will be on hiatus till the middle of next week.
Here’s a few items of note that came across the virtual wire over the last few days.
Mylan’s EpiPen Disaster.
In the story-that-will-not-die, EpiPen manufacturer Mylan continues to dig its hole deeper and deeper. The latest news – the actual cost to make and fill an EpiPen is less than 10% of the product’s actual price. And may be as low as four bucks – for a $300 injector.
Of course, when you need an EpiPen, you really, really need one – and could not care less what it costs. (it is used to reverse the most dangerous symptom of anaphylactic shock – asphyxiation)
But there are so many hands out in the EpiPen distribution chain, all making a margin as the product works its way down to the end user. Most striking is the rebate Mylan likely pays to the insurer – one estimated by the estimable Adam Fein at around 40% of the product’s list price.
Now Mylan CEO Heather Bresch is providing all of us a lesson in how NOT to respond when confronted by reporters asking about price increases and huge compensation packages. Bresch said, and I quote: “No one’s more frustrated than me.”
That takes some balls – and a whole lot of cluelessness.
The parents who can’t afford to replace their kids’ EpiPens every year when they expire and have high-deductible plans so they pay the $600 out of pocket might be a touch more “frustrated” than Ms. $19-million-a-year Bresch.
Beyond that, there’s a nastier, uglier, and way bigger problem here. Health care in this country is a for-profit business, and Mylan is operating in the best interests of its stockholders.
And no, the “free market” won’t solve this issue – markets don’t care about people.
Provider consolidation continues
CMS’ changes in reimbursement are driving adoption of IT systems designed to track and report patient encounters with a focus on quality metrics. These systems are expensive, difficult to implement, and require ongoing updating and maintenance.
More consolidation does not mean more efficiency or cost-effectiveness…in fact some data indicates costs go up.
Implication – more sophistication in billing, electronic medical records (EMR), coding and contracting means payers will find smarter and more knowledgeable negotiators across the table, and more sophisticated billing.
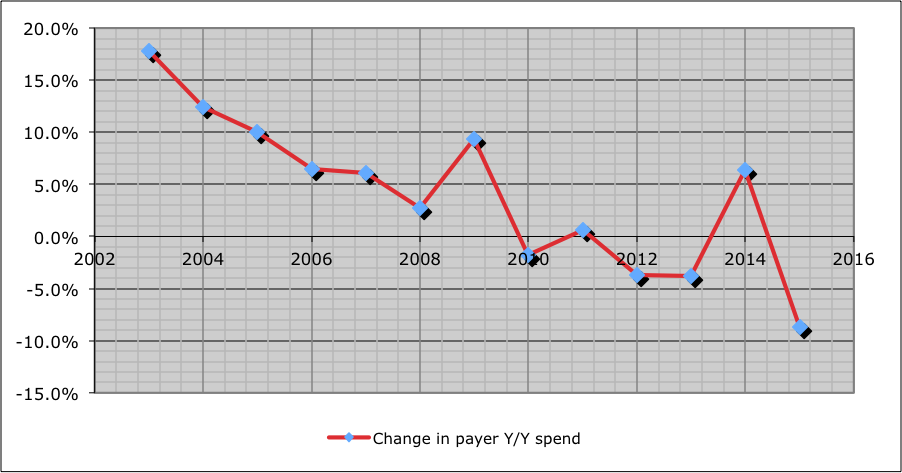
Work comp rates keep coming down
California, North Carolina, Kentucky, Tennessee all are joining the states that have announced decreased work comp rates. I know Florida’s getting all Sunshine-y for plaintiff attorneys, and payers are in a justifiable uproar about that, but that’s an anomaly.
Implications – good news for employers and taxpayers, bad news for opt-out.
Which remains a “solution” (and a pretty poor one at that” to a problem that doesn’t exist.
Okay, gotta run. see you next week!